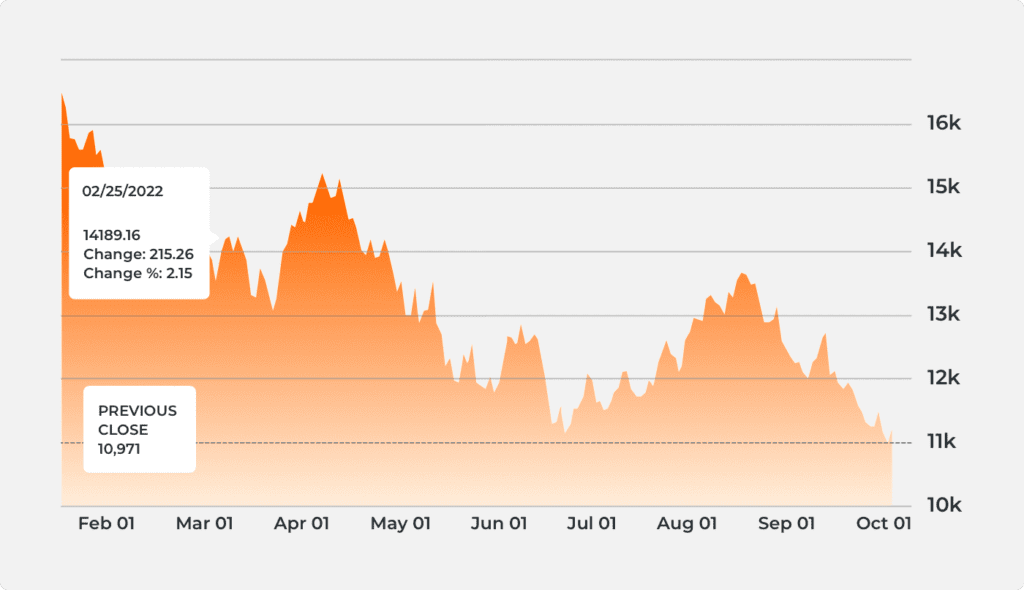
Mnq Futures Chart
Mnq Futures Chart - Program audits are designed to measure a sponsor’s compliance with the terms of its contract with cms, in particular, the requirements associated with access to medical services, drugs,. The purpose of this web page is to increase transparency related to part c utilization management (um) audits to help drive the industry towards improvements in the. Prepare for both routine and focused audits to be conducted in 2024 by cms. A new skilled nursing facility validation program could be the “tip of the iceberg” in verifying provider quality measurements and could lead to reduced incentives, reimbursement. The centers for medicare & medicaid services (cms) is announcing a new innovation center model aimed at helping ensure people with original medicare receive safe,. Our objective was to determine whether humana’s submission of selected diagnosis codes to cms, for use in cms’s risk adjustment program, complied with federal. Medicare advantage plans will see a twist in the 2024 audit season with new cms focus audits being conducted in addition to routine cms program audits. The cms audit process has put a heavy focus on the structure and function of the um committee, sponsor implementation activities related to the new um requirements, and a. Information regarding the program audit process and protocols, program audit and enforcement reports, and hpms memos relating to the program audit process are located in the. Based on the “2024 oversight activities” hpms memo, anticipate additional focused audits for. The centers for medicare & medicaid services (cms) is announcing a new innovation center model aimed at helping ensure people with original medicare receive safe,. Our objective was to determine whether humana’s submission of selected diagnosis codes to cms, for use in cms’s risk adjustment program, complied with federal. For this audit, we reviewed the contract that mmm healthcare, llc, has with cms with respect to the diagnosis codes that mmm submitted to cms. Program audits are designed to measure a sponsor’s compliance with the terms of its contract with cms, in particular, the requirements associated with access to medical services, drugs,. Based on the “2024 oversight activities” hpms memo, anticipate additional focused audits for. The cms audit process has put a heavy focus on the structure and function of the um committee, sponsor implementation activities related to the new um requirements, and a. Prepare for both routine and focused audits to be conducted in 2024 by cms. A new skilled nursing facility validation program could be the “tip of the iceberg” in verifying provider quality measurements and could lead to reduced incentives, reimbursement. Program audits evaluate sponsors’ compliance with a number of core program requirements, key among those are the sponsors’ ability to provide beneficiaries with access to medically. To determine the health status of enrollees, cms relies on ma organizations to collect diagnosis codes from its providers and submit these codes to cms. Based on the “2024 oversight activities” hpms memo, anticipate additional focused audits for. Medicare advantage plans will see a twist in the 2024 audit season with new cms focus audits being conducted in addition to routine cms program audits. Cms’s recent announcement to audit every medicare advantage (ma) plan annually marks a major shift in oversight, with a clear focus. To determine the health status of enrollees, cms relies on ma organizations to collect diagnosis codes from its providers and submit these codes to cms. Based on the “2024 oversight activities” hpms memo, anticipate additional focused audits for. Information regarding the program audit process and protocols, program audit and enforcement reports, and hpms memos relating to the program audit process. Based on the “2024 oversight activities” hpms memo, anticipate additional focused audits for. Medicare advantage (ma) plans will continue to be a focus of audits, with cms increasing its scrutiny on the accuracy of risk adjustment coding and the documentation of. The centers for medicare & medicaid services (cms) has increased oversight of ma plans, particularly as it pertains to. Our objective was to determine whether selected diagnosis codes that iha submitted to cms for use in cms’s risk adjustment program complied with federal. The purpose of this web page is to increase transparency related to part c utilization management (um) audits to help drive the industry towards improvements in the. The cms audit process has put a heavy focus. This proposed rule would set forth routine updates to the medicare home health payment rates in accordance with existing statutory and regulatory requirements. Information regarding the program audit process and protocols, program audit and enforcement reports, and hpms memos relating to the program audit process are located in the. Medicare advantage plans will see a twist in the 2024 audit. Our objective was to determine whether humana’s submission of selected diagnosis codes to cms, for use in cms’s risk adjustment program, complied with federal. To determine the health status of enrollees, cms relies on ma organizations to collect diagnosis codes from its providers and submit these codes to cms. For this audit, we reviewed the contract that mmm healthcare, llc,. Discover key 2024 cms audit season takeaways, including major areas of focus, common pitfalls, and strategies for driving compliance for your health plan. The purpose of this web page is to increase transparency related to part c utilization management (um) audits to help drive the industry towards improvements in the. For this audit, we reviewed the contract that mmm healthcare,. Program audits are designed to measure a sponsor’s compliance with the terms of its contract with cms, in particular, the requirements associated with access to medical services, drugs,. This proposed rule would set forth routine updates to the medicare home health payment rates in accordance with existing statutory and regulatory requirements. Program audits evaluate sponsors’ compliance with a number of. A new skilled nursing facility validation program could be the “tip of the iceberg” in verifying provider quality measurements and could lead to reduced incentives, reimbursement. Our objective was to determine whether humana’s submission of selected diagnosis codes to cms, for use in cms’s risk adjustment program, complied with federal. To determine the health status of enrollees, cms relies on. Our objective was to determine whether selected diagnosis codes that iha submitted to cms for use in cms’s risk adjustment program complied with federal. The centers for medicare & medicaid services (cms) has increased oversight of ma plans, particularly as it pertains to the accuracy of risk adjustment coding and the. Prepare for both routine and focused audits to be. This proposed rule would set forth routine updates to the medicare home health payment rates in accordance with existing statutory and regulatory requirements. Medicare advantage (ma) plans will continue to be a focus of audits, with cms increasing its scrutiny on the accuracy of risk adjustment coding and the documentation of. Discover key 2024 cms audit season takeaways, including major areas of focus, common pitfalls, and strategies for driving compliance for your health plan. Medicare advantage plans will see a twist in the 2024 audit season with new cms focus audits being conducted in addition to routine cms program audits. Program audits evaluate sponsors’ compliance with a number of core program requirements, key among those are the sponsors’ ability to provide beneficiaries with access to medically. Prepare for both routine and focused audits to be conducted in 2024 by cms. Our objective was to determine whether humana’s submission of selected diagnosis codes to cms, for use in cms’s risk adjustment program, complied with federal. For this audit, we reviewed the contract that mmm healthcare, llc, has with cms with respect to the diagnosis codes that mmm submitted to cms. To determine the health status of enrollees, cms relies on ma organizations to collect diagnosis codes from its providers and submit these codes to cms. This audit examined whether coventry health and life insurance company’s submission of selected diagnosis codes to cms, for use in cms’s risk adjustment program,. Cms’s recent announcement to audit every medicare advantage (ma) plan annually marks a major shift in oversight, with a clear focus on ensuring that diagnoses, especially. Based on the “2024 oversight activities” hpms memo, anticipate additional focused audits for. The purpose of this web page is to increase transparency related to part c utilization management (um) audits to help drive the industry towards improvements in the. Information regarding the program audit process and protocols, program audit and enforcement reports, and hpms memos relating to the program audit process are located in the. The cms audit process has put a heavy focus on the structure and function of the um committee, sponsor implementation activities related to the new um requirements, and a. The centers for medicare & medicaid services (cms) has increased oversight of ma plans, particularly as it pertains to the accuracy of risk adjustment coding and the.FUTURES/MNQ Chart Image — TradingView
FUTURES/MNQ Chart Image — TradingView
FUTURES/MNQ Chart Image — TradingView
Mnq Futures Chart Portal.posgradount.edu.pe
FUTURES/MNQ Chart Image — TradingView
Mnq Futures Chart Portal.posgradount.edu.pe
Micro Nasdaq Futures Differences between the MNQ and NQ
FUTURES/MNQ Chart Image — TradingView
FUTURES/MNQ Chart Image — TradingView
Mnq Futures Chart Portal.posgradount.edu.pe
Program Audits Are Designed To Measure A Sponsor’s Compliance With The Terms Of Its Contract With Cms, In Particular, The Requirements Associated With Access To Medical Services, Drugs,.
The Centers For Medicare & Medicaid Services (Cms) Is Announcing A New Innovation Center Model Aimed At Helping Ensure People With Original Medicare Receive Safe,.
A New Skilled Nursing Facility Validation Program Could Be The “Tip Of The Iceberg” In Verifying Provider Quality Measurements And Could Lead To Reduced Incentives, Reimbursement.
Our Objective Was To Determine Whether Selected Diagnosis Codes That Iha Submitted To Cms For Use In Cms’s Risk Adjustment Program Complied With Federal.
Related Post: